How the Microbiome Helps – and Sometimes Hurts – the Immune System
At the heart of the human immune system lies a paradox. One of its main functions is to protect the body from harmful foreign substances, including viruses and bacteria. Yet scientists have discovered that these same microbes are also the immune system’s closest ally.
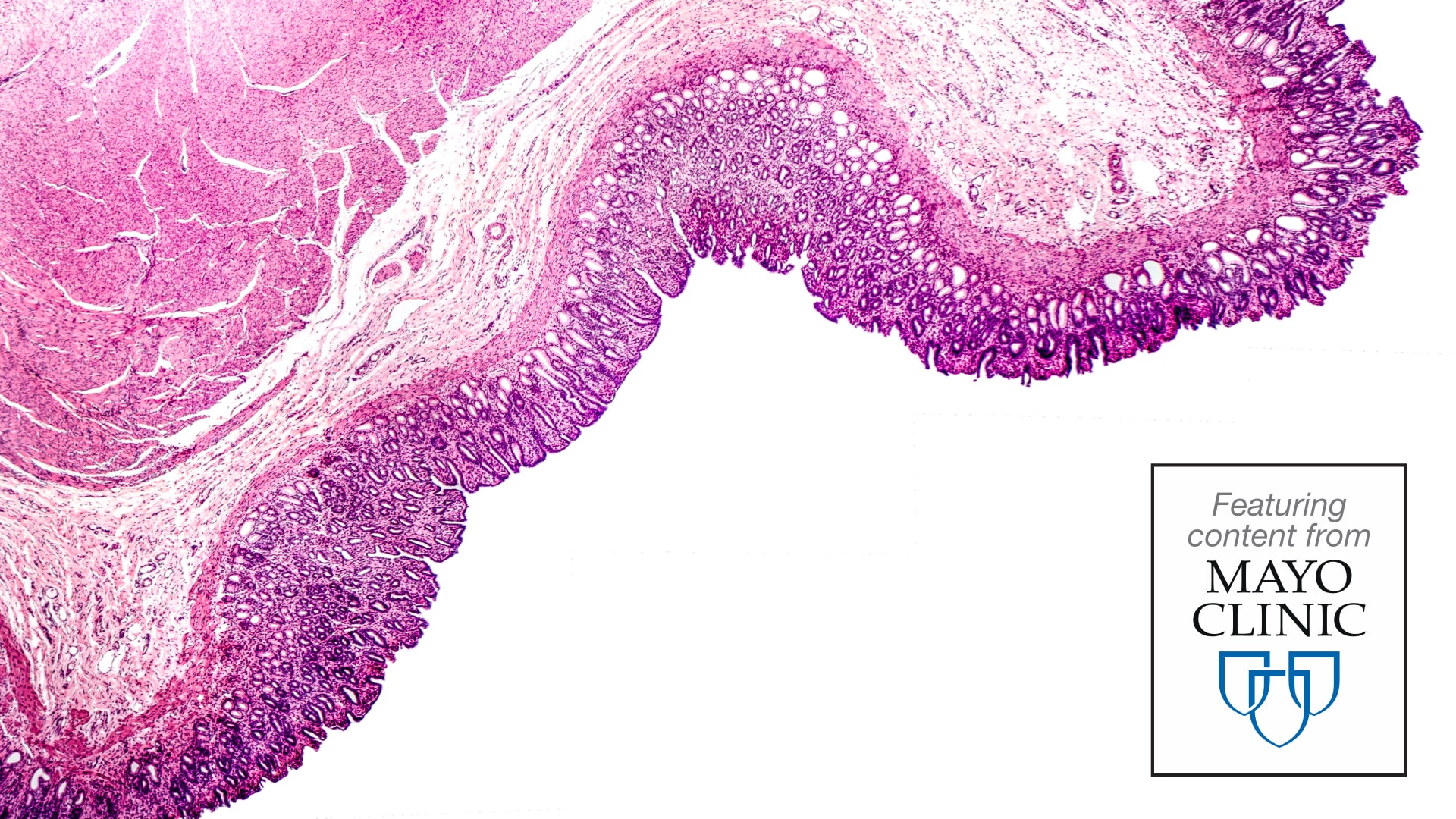
Although the immune system is designed to fight and destroy harmful bacteria and other microbes, the human body also teems with microbes that share a mutually beneficial relationship with their host. In fact, microbes might outnumber the cells in the body.1,2 From early childhood on, hundreds of different microbes naturally colonize the gut, skin, and other parts of the body that interact with the outside world.
The body's microorganisms, along with all their genes, are together known as the microbiome. The microbes that live in a particular environment, such as the digestive tract, are referred to as microbiota.3
Both humans and their microbes benefit from each other. For example, the microbiome provides many beneficial substances to the body, including vitamin K, which is important for blood clotting and bone health.4 The microbiota also works closely with the immune system. What researchers are learning about the microbiome could have implications for allergies, asthma, and other immune disorders.
Microorganisms, disease, and health
In the 19th century, scientists discovered that certain microorganisms cause disease. As a result, people began taking steps to sanitize their environments, such as sewage management, hand washing, and pasteurization.
The development of antibiotics and vaccines to treat and prevent infectious diseases dramatically decreased mortality from many diseases, especially in children, and human life span increased. More recently, however, another puzzle has emerged as conditions related to immune system dysregulation, such as allergies and asthma, appear to be increasing.
In 1989, epidemiologist David Strachan proposed an idea that is known as the "hygiene hypothesis." It suggests that a modern, industrialized lifestyle, with smaller families, fewer animals, and less dirt, reduces exposure to microbes, especially in children.
Although this generally results in less infectious disease, it might also affect immune system development.5 A less robust immune system can leave an individual more prone to allergies, asthma, and eczema, and possibly even obesity, diabetes, and autoimmune diseases.6-9
So what’s going on?
The microbiota and immune system development
Scientists have tackled this dilemma by studying germ-free mice, which have no gut bacteria. The immune system in these mice is weak and incomplete. When researchers introduce microbes – sometimes even a single type of bacteria – into germ-free mice they can develop a fully functional immune system.10
In humans as well, microbes play a critical role in shaping the immune system from the earliest stages of development. Even before birth, a baby begins to acquire resident populations of foreign organisms.11-13
The manner of birth also affects the microbiota. Caesarean (C section) birth – by nature more sterile than natural childbirth – frequently leads to different, often less diverse microbes in the infant gut compared to babies born vaginally.
A diverse microbiota primes the immune system, allowing it to differentiate between good and bad bacteria and hence do its job of recognizing and fighting harmful invaders.7
Greater diversity equals a stronger immune system
A lack of diversity in bacterial species can influence the development of immune related disorders, such as allergies and asthma.6,8,9,14 Specific types of microbes are linked to overactive immune responses (asthma, allergies, and eczema) or greater tolerance of environmental challenges.8 For example, children with eczema often have smaller quantities and less diversity of healthy gut bacteria.7
Researchers hope that a greater understanding of the role of the microbiota in immune development will open new strategies to reduce immune deficiencies and treat or prevent autoimmune diseases such as inflammatory bowel disease and type 1 diabetes.15
For example, some evidence suggests that when women take a probiotic supplement during pregnancy and the first six months of infancy, their babies have a lower likelihood of developing eczema.7
Of course, much more work remains to be done to fully understand the relationships between the microbiome, the immune system, and disease. But the outlook for discovering new ways to influence immune system development and enhance health is promising.
References
- Sender R, Fuchs S, Milo R. Are we really vastly outnumbered? Revisiting the ratio of bacterial to host cells in humans. Cell 2016;164:337-340.
- Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol 2016;1-14.
- Quigley E. Basic definitions and concepts: Organization of the gut microbiome. Gastroenterology Clin North Am 2017;46:1-8.
- Chen Y-C, Greenbaum J, Shen H, et al. Association between gut microbiota and bone health: Potential mechanisms and prospective. J Clin Endocrinol Metab 2017;102(10):3635-3646.
- Strachan D. Hay fever, hygiene, and household size. BMJ 1989;299(6710):1259-1260.
- Seroogy C, Prescott S. Ontogeny of immune development and its relationship to allergic diseases and asthma. In: Middleton's Allergy: Principles and Practice. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. [Accessed Jan. 23, 2020.]
- Pothmann A, Illing T, Wiegand C, et al. The microbiome and atopic dermatitits: A review. Am J Clin Dermatol 2019;20:749-761.
- Chernikova D, Yuan I, Shaker M. Prevention of allergy with diverse and healthy microbiota: An update. Current Opin Pediatr 2019;31(3):418-425.
- Lee J, Kim C, Ramakrishnan V. Microbiome and disease in the upper airway. Curr Opin Allergy Clin Immunol 2019;19(1):1-6.
- O'Hara A, Shanahan F. The gut flora as a forgotten organ. EMBO Rep 2006;7(7):688-693.
- Kim H, Sitarik A, Woodcroft K, et al. Birth mode, breastfeeding, pet exposure, and antibiotic use: Associations with the gut microbiome and sensitization in children. Curr Allergy Asthma Rep 2019;19:22.
- Hill C, Lynch D, Murphy K, et al. Evolution of gut microbiota composition from birth to 24 weeks in the INFANTMET cohort. Microbiome 2017;5:4.
- Francino M. Birth-mode-related differences in gut microbiota colonization and immune system development. Ann Nutr Metab 2018;73(suppl 3):12-16.
- Adeyeye T, Yeung E, McLain A, et al. Wheeze and food allergies in children born via cesarean delivery: The Upstate KIDS Study. Am J Epidemiol 2019;188(2):355-362.
- Goronzy J, Gustafson C, Weyand C. Immune deficiencies at the extremes of age. In: Rich R, Fleisher T, Shearer W, et al. Clinical Immunology: Principles and Practice. 5th ed. Elsevier; 2019. https://www.clinicalkey.com. Accessed Jan. 23, 2020.


 This site is exclusive to Thorne Retail customers.
This site is exclusive to Thorne Retail customers.